Big Toe, Big Problems
Today’s guest post comes from Cressey Sports Performance colleague, Dr. James Spencer. Enjoy! -EC
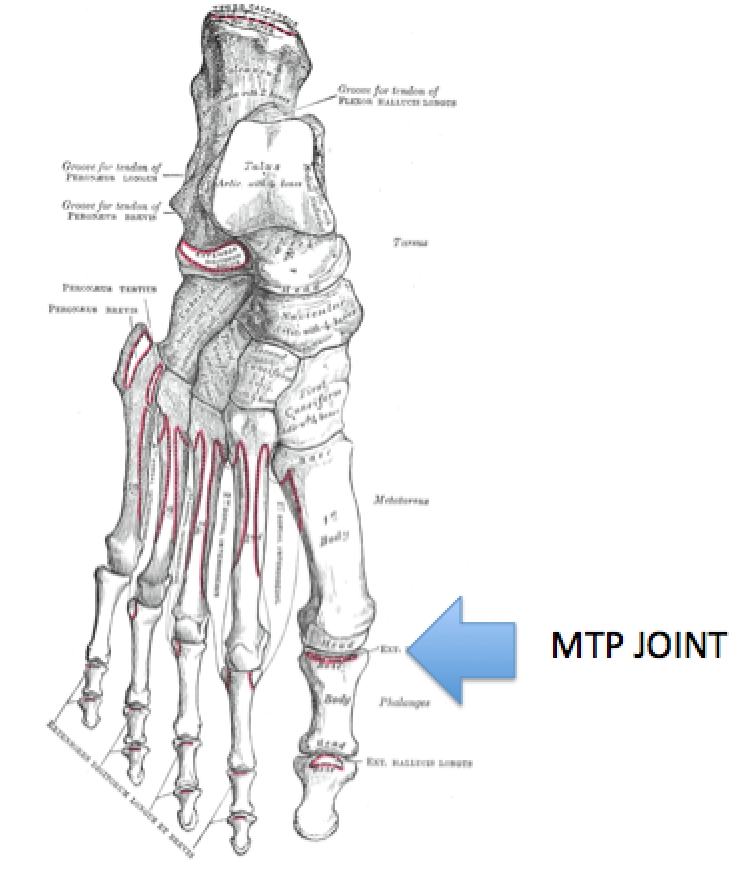
Epidemiological research suggests that the incidence of foot problems, specifically issues with the first metatarsalphalangeal joint (MTP) is common (1). These common big toe and foot problems are exposed in the systematic approach of the Selective Functional Movement Assessment (SFMA) and Functional Movement Screen (FMS). The big toe condition I would like to highlight is Functional Hallux Limitus (FHL). FHL is a separate distinct diagnosis from Structural Hallux Limitus (SHL). FHL is characterized by a lack of dorsiflexion of the first MTP joint during the gait cycle only (2).
The one problem that I typically see with this condition is how infrequently diagnosed it is. The reason for this may be that patients may not have experienced pain in their toe or a drastic compensation pattern. Additional research also reported that the presence in foot symptoms does not necessarily correlate with the presence of dysfunction and that patients may be experiencing dysfunction without having any accompanying symptoms (1).
The big toe is a very underestimated player in the Joint by Joint Theory. Popularized by Gray Cook and Mike Boyle, the Joint by Joint approach is alternating series of stable segments on mobile joints, where (generally):
1st MTP: Needs Mobility
Mid-Foot: Needs Stability
Ankle: Needs Mobility
Knee: Needs Stability
Hip: Needs Mobility
Lumbar Spine: Needs Stability
Thoracic Spine: Needs Mobility
Cervical Spine (lower): Needs Stability
Cervical Spine (upper): Needs Mobility
Shoulder: Needs Mobility
Elbow: Needs Stability
Wrist: Needs Mobility
You could see how an alteration in this Joint by Joint approach could affect the mechanics and joints up and down the kinetic chain. In this article I would like to explore FHL and its interplay with Regional Interdependence, which refers to the concept that seemingly unrelated impairments in a remote anatomical region may contribute to, or be associated with, the patient’s primary complaint (3). Therefore, you could see how a lack of big toe mobility can lead to a wide spread of conditions locally, at the joint, and systemically, up the kinetic chain and beyond. For example, some associated signs and conditions may include overpronation, ankle mobility restrictions, toe out posture, posterior tibialis tendinosis, achilles tendinosis, plantar fasciitis and patellar tendinosis, just to name a few. Regional interdependence displays the amazing anatomical and biomechanical interconnection throughout the human body.
Functional Anatomy
The first metatarsal is the shortest and thickest of the metatarsals. Two sesamoid bones, encased in the tendons of the intrinsic muscles, lie beneath the head of the first metatarsal. Suggested sesamoid function for the first metatarsal allows the big toe to plantar flex during extension of the hallux, enhance the load-bearing capacity of the first metatarsal, and to improve the mechanical leverage for the attached intrinsic muscles (4). Depending on the literature you read, the first ray is designed for 50-70 degrees of big toe extension during static evaluation. However, I would argue that 45 degrees of big toe extension is actually adequate during the gait cycle. This is supported with the work of Nawoczenski in the Journal of Bone and Joint Surgery. I could not find any published research on if these values were different during the running cycle. If you look at Thomas Myers’ work with the Superficial Back Line (SBL), you can see how the lack of big toe extension could wreak havoc on the entire kinetic chain via regional interdependence.
Originating from the plantar aspect of the calcaneus, the plantar fascia is more than just a passive band of connective tissue. As the plantar fascia travels distally towards the toes, it separates into five slips of fascia. Each plantar fascia slip inserts plantarly onto each of the five digits. As the foot transitions from midstance into push-off, the toes begin to dorsiflex and the plantar fascia is activated. This activation of the plantar fascia upon hallux dorsiflexion is referred to as the “windlass mechanism” and is the second step in preparing the foot for propulsion.

Since power during propulsion is dependent upon the foot’s ability to become a rigid lever, ensuring proper hallux dorsiflexion during the gait is key to achieving full foot supination (5). Considering that during gait, the entire body is advancing past this single joint, the ability to dorsiflex, and subsequently raise the heel during single support phase while simultaneously supporting against the developing forces for forward motion is essential for normal, efficient gait. If this mechanism fails, sagittal plane compensation will be forced to occur (6). When the first MTP joint motion is disrupted enough to prevent stabilization of the foot structure during maximal hallux dorsiflexion, through the effect of the windlass mechanism, then normal foot stabilization during propulsion is disrupted, and becomes clinically significant (7).
Aside from the specific biomechanics that are addressed in the lower quarter, looking at mobility loss more globally will always relate to an anterior weight shift. Repetitive function with an anterior weight shift yields facilitation and inhibition in a very predictable pattern.
Common Compensations with FHL
Compensations will occur due to injuries, faulty mechanics and previous experiences. We have to take a step back and realize our CNS (Central Nervous System) is a high-speed train moving forward with “Life;” therefore, compensations will inevitably occur throughout our lives. We could blame previous injuries, posture, ergonomics, it really doesn’t matter what we point the finger at, but our CNS will continue to move forward whether the movement is mechanically advantageous to us or not. The key is not allowing compensatory patterns to become engraved as movement patterns. The CNS loves stimulation and constant feedback for neuroplasticity.
This video displays amazing neurological changes and shows how habits, movement patterns and previous experiences influence our neurological systems. Plus, you have to appreciate the MacGyver Mullet comment! I also want this to be an eye opener for people to see how long it can take to learn new motor skills and how easily it is to revert right back in to an old pattern.
Some of the most common compensations that I see consist of limited proprioception in the midfoot, limited ankle mobility, and limited hip extension. Limited proprioception in the midfoot can lead to plantar fascitis or medial arch stress. Limited ankle mobility – typically dorsiflexion – is another common imbalance that must be assessed in a client seeking power at propulsion. Normal gait requires at least 10 degrees of ankle dorsiflexion with maximum ankle dorsiflexion occurring during late midstance. Limited ankle mobility can lead to a myriad of compensations including midfoot pronation, knee hyperextension and an early heel rise during gait (5). Limited hip extension can lead to abduction compensation and produce the classic overpronated foot type and abducted stance position. The stride length shortens and reduces hip extension and glute activation. As Charlie Weingroff has noted, this is caused when the correct pathway of motion is blocked by the lack of 1st ray dorsiflexion, the person will produce an abducted foot in order to roll off the inside of the toe in order to allow for hip extension (8). I find that this compensation is most often related to the development of Hallux Valgus and bunion formation.
Corrective Strategies
Here’s one of my favorite simple drills to use (in combination with manual therapy) with folks with FHL:
I also like to progress individuals to 2×4 walks to integrate this pattern in balance training:
Final Thoughts
Your big toe is essential for proper balance, running, walking and many other athletic activities or exercises. As the foundation to human movement, optimal power during propulsion is dependent upon proper foot posture and muscle activation patterns. With every step, the human foot must convert from a mobile adaptor at midstance to a rigid lever for propulsion. Integrating foot-specific exercises sets the foundation for sufficient foot strength and forefoot re-supination. The quicker the foot can become a rigid lever, the greater the power that is unleashed during propulsion (5). I believe that there is inadequate diagnostic criteria for clinicians to properly diagnose FHL. Since FHL is diagnosed during closed kinetic chain, we should look in to a more definitive way to diagnose this functional condition. Moreover, a dynamic gait analysis that shows timing and pressure differences in the foot may be a good source of objective measurement for future diagnostic criteria.
My goal of this article is to raise awareness of how important the big toe mobility and stability is for every day life and function. Please don’t take the movement algorithm of walking for granted because it is one of the most complex movements the human body performs. Let this final picture be a reminder to never chase pain when evaluating or treating someone and keep the thought of regional interdependence in mind.
Note: references for this article will be posted as the first comment below.
About the Author
 Based in South Florida, Dr. James Spencer is a Sports Performance Chiropractor, Certified Athletic Trainer, and Fellow of the International Academy of Medical Acupuncture. He has formal training in Active Release Techniques, Graston Technique, Kinetacore Functional Dry Needling, SpiderTech Kinesiology Tape, RockTape Fascial Movement Taping, Postural Restoration Institute, Y-Balance Test, FMS, SFMA, Mike Boyle’s Certified Functional Strength Coach and the Onnit Academy of Unconventional Training. You can find Dr. Spencer on Facebook, Instagram and at www.DrJamesSpencer.com.
Based in South Florida, Dr. James Spencer is a Sports Performance Chiropractor, Certified Athletic Trainer, and Fellow of the International Academy of Medical Acupuncture. He has formal training in Active Release Techniques, Graston Technique, Kinetacore Functional Dry Needling, SpiderTech Kinesiology Tape, RockTape Fascial Movement Taping, Postural Restoration Institute, Y-Balance Test, FMS, SFMA, Mike Boyle’s Certified Functional Strength Coach and the Onnit Academy of Unconventional Training. You can find Dr. Spencer on Facebook, Instagram and at www.DrJamesSpencer.com.